Importance Of Baseline Tumor Cell Assessment In Treatment Planning
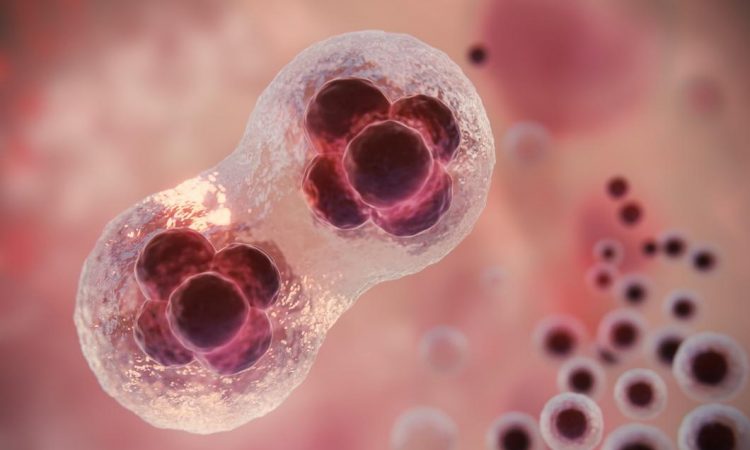
Baseline tumor cell assessment is crucial for developing effective cancer treatment plans. It offers a comprehensive understanding of tumor characteristics, allowing medical professionals to make informed decisions about the most suitable treatment options. By analyzing tumor cells’ genetic and molecular makeup, oncologists can gain insights into the cancer’s aggressiveness, growth rate, and potential for metastasis, which are essential for determining the appropriate course of action.
This assessment is critical in personalized medicine, where treatment is tailored to the individual’s unique cancer profile. A one-size-fits-all approach is often ineffective, so understanding each tumor’s specific characteristics helps craft a treatment plan that maximizes the chances of successful outcomes. Personalized care focuses on the tumor’s unique molecular and genetic profile rather than a generic protocol, enhancing the effectiveness of the treatment.
Additionally, baseline tumor cell assessment can identify potential biomarkers that indicate the tumor’s response to various therapies. This information helps explore targeted therapies that may be more effective for the specific type of cancer. It also guides the selection of appropriate chemotherapeutic agents, radiation therapy, or a combination of modalities, ensuring that the patient receives the most effective and personalized care possible.
Methods And Techniques For Baseline Tumor Cell Assessment
Baseline tumor cell assessment uses various methods to understand a tumor’s characteristics. Biopsies, such as fine-needle aspiration, core biopsy, or surgical biopsy, obtain tumor samples for analysis.
Essential techniques include immunohistochemistry (IHC) to detect specific proteins and assess tumor growth, aggressiveness, and metastasis potential. Advanced methods like next-generation sequencing (NGS) analyze the tumor’s genetic profile for mutations and alterations. Liquid biopsy, a non-invasive option, examines circulating tumor cells or DNA in the bloodstream to monitor the cancer over time.
Role Of Baseline Tumor Cell Assessment In Determining Prognosis
Baseline tumor cell assessment is crucial for determining cancer prognosis. By examining tumor characteristics, medical professionals can predict disease progression and treatment response.
Key factors include tumor grade, with higher-grade tumors indicating a poorer prognosis. Techniques like IHC help assess tumor grade and overall outlook.
Identifying genetic mutations or protein expressions, such as HER2 in breast cancer or BRAF V600E in melanoma, provides insight into disease aggressiveness and prognosis. This information enables oncologists to tailor treatment plans effectively.
Impact Of Baseline Tumor Cell Assessment On Treatment Decisions
Baseline tumor cell assessment profoundly impacts oncologists’ treatment decisions by revealing the unique characteristics of a patient’s cancer and predicting therapy responses.
This assessment identifies targeted therapies by uncovering genetic and molecular tumor details, allowing for personalized, effective, and less toxic treatments than traditional chemotherapy.
It also guides the selection of suitable chemotherapeutic agents and combinations, ensuring optimal effectiveness. Additionally, it helps identify potential resistance mechanisms, enabling proactive adjustments to the treatment plan for better outcomes.
Case Studies Highlighting The Impact Of Baseline Tumor Cell Assessment
The impact of baseline tumor cell assessment on treatment planning is evident in real-world cases.
In one case, a 55-year-old with stage III non-small cell lung cancer (NSCLC) had a biopsy revealing the EGFR T790M mutation. This led to the targeted therapy of osimertinib, resulting in significant tumor reduction.
Another case involved a 42-year-old with triple-negative breast cancer (TNBC). Baseline assessment revealed a BRCA1 mutation, guiding a treatment plan with chemotherapy and a PARP inhibitor, which significantly reduced the tumor and prevented metastasis.
These examples show how baseline tumor cell assessment informs targeted therapies, improving patient outcomes and personalizing cancer care.
Challenges And Limitations Of Baseline Tumor Cell Assessment
Baseline tumor cell assessment is vital for cancer treatment planning but faces challenges and limitations.
Tumor cell heterogeneity complicates obtaining a comprehensive understanding from a single biopsy, and tumors can evolve genetically, especially with treatment.
Some techniques, like surgical biopsy, are invasive and carry risks, and advanced diagnostics like NGS and liquid biopsy may not be widely available, particularly in low-resource areas.
Interpreting results requires specialized expertise; errors can lead to suboptimal treatment and adverse patient outcomes.
Advances In Baseline Tumor Cell Assessment Technology
Despite challenges, technological advancements are enhancing the accuracy and accessibility of baseline tumor cell assessment in cancer care.
Notable progress includes liquid biopsy, which analyzes circulating tumor cells or DNA in the bloodstream—this provides tumor insights without traditional biopsies and allows for ongoing monitoring.
AI and machine learning advancements help analyze complex genetic data, identify patterns and biomarkers, and guide targeted therapies for personalized treatment.
Integrating baseline tumor cell assessment with imaging and genomic profiling offers a comprehensive understanding of the tumor, leading to more informed and effective treatment decisions.
Integrating Baseline Tumor Cell Assessment Into Personalized Treatment Plans
Integrating baseline tumor cell assessment into cancer treatment plans necessitates close collaboration between oncologists, pathologists, and other healthcare professionals. By standardizing the biopsy and assessment process with advanced diagnostics, we ensure timely and accurate information to guide treatment decisions.
Prompt diagnosis is crucial for identifying the most effective treatment plan. At Carolina Urgent Care, effective communication of assessment findings to patients and the healthcare team is essential for building trust and facilitating shared decision-making. Ongoing monitoring and reassessment of tumor characteristics allow for adapting treatment plans to the patient’s evolving needs, optimizing outcomes, and enhancing the quality of cancer care.
Conclusion: Future Directions In Baseline Tumor Cell Assessment And Treatment Planning
Baseline tumor cell assessment will be crucial in personalized cancer treatment. Advances in diagnostics will improve its accuracy and accessibility, enabling better treatment decisions. Integrating genetic, molecular, and clinical data will provide a comprehensive tumor understanding, leading to more personalized strategies.
Exploring new biomarkers and therapeutic targets will further personalize care. Standardizing data collection and analysis will ensure widespread adoption, optimizing patient outcomes and quality of life.
In summary, baseline tumor cell assessment empowers oncologists to make informed decisions, significantly improving patient outcomes and remaining vital as cancer care evolves.